Natural birth methods and techniques are becoming more and more popular amongst women who are choosing to have hospital deliveries. As women become more educated and aware of their choices regarding pain management, interventions and delivery, they are also learning more about their postpartum care options as well. Placentophagia, or the act of consuming one's placenta after delivery, is starting to be less of a fringe activity and more mainstream for mothers who are looking for natural alternatives for hormone, mood and physical recovery in the postpartum period.
Natural birth methods and techniques are becoming more and more popular amongst women who are choosing to have hospital deliveries. As women become more educated and aware of their choices regarding pain management, interventions and delivery, they are also learning more about their postpartum care options as well. Placentophagia, or the act of consuming one's placenta after delivery, is starting to be less of a fringe activity and more mainstream for mothers who are looking for natural alternatives for hormone, mood and physical recovery in the postpartum period. What exactly is placentophagia?
Simply put placentophagia is the act of mammals eating their placentas after the birth of their young. Almost all species of mammals, with the exception of humans, routinely practice placentophagia. There are hormones present in the placenta, namely prostaglandin and oxytocin, that may help shrink the uterus down to it's pre-pregnancy size. This combined with the need to hide anything that may attract predators near a new mother and their young is why most mammals engage in this activity. Humans have little to no fear of predation while recovering from birth, which is one of the speculated reasons that we no longer have the urge to consume our placentas right after delivery.
Why would I want to eat my placenta?
While there have been no studies showing the benefits of placentophagia in humans there is an overwhelming amount of anecdotal evidence to be found from women who have ingested their placentas in the form of capsules, tinctures, edibles or even raw. The most commonly reported benefits of placentophagia are:
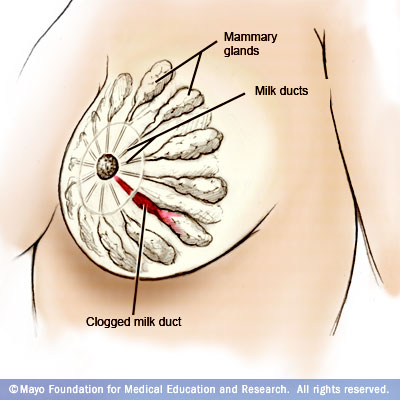
- Increased milk production
- Shortened recovery time postpartum
- Decreased postpartum bleeding
- Anxiety and stress relief
- Increased energy
- Decreased Baby Blues symptoms
- Decreased Postpartum Depression symptoms
How does placenta encapsulation work?
Most women are put off by the thought of even looking at their placenta, let alone blending it in to a postpartum smoothie. That is where placenta encapsulation comes in. A professional with special training or experience will come and collect your placenta shortly after you deliver. They will then transport it to their home or office where they have set up a hygienic space to process and encapsulate placentas. Alternatively if you have a home birth they may even process it in your own home if you so desire. After transportation, they will prepare the placenta for dehydration, dehydrate it and then grind it into a fine powder. The powder is then placed in to capsules which are ready for you to take as needed for postpartum symptom support and relief.
What are the risks?
The CDC (Centers For Disease Control) and ACOG (American College of Obstetricians and Gynecologists) do not recommend the practice of placentophagia in the form of placenta encapsulation (or any other form, for that matter). Why is this when there have been few to no studies showing risks to the practice?
As of now, there are NO REGULATIONS for those who offer placenta encapsulation or processing services. That means that there are no safety or hygiene standards that they must adhere to when handling your placenta. This is a problem because the placenta is a blood-rich organ - if health and safety standards are not practiced where placentas from multiple women are processed the risk for blood-borne and food illness increases significantly. It is vital if you are considering having your placenta encapsulated that the professional you hire practices safety and hygiene protocols to help minimize this risk. Things to ask the professional who is encapsulating your placenta are:
- Do you thoroughly disinfect all of your bowls, tools, equipment and workspace after each placenta? *Note: This does not mean using warm water and an antibacterial dish soap! A proper bleach solution or something similar must be used.
- How soon after my delivery can you come and retrieve my placenta? **Note: Most hospitals require that if you are taking your placenta home, you must have it picked up no more than between 1 and 4 hours after delivery. Check with your hospital regarding their policies.
- Where and how do you store placentas for transport and/or placentas waiting to be processed? ***Note: Like any sort of organ intended for consumption, your placenta must be stored in a cool, dry and clean container or frozen if not used right away. If the person transporting your placenta is bringing their own cooler, make sure they disinfect the cooler with a bleach solution between each client.
It is important to note that you should never ingest placenta capsules, tinctures or edibles derived from another woman's placenta. This greatly increases your and your baby's risk for blood-borne illness.
Other risks include unwanted side effects. Again, there are no studies showing adverse side effects from placentophagia. Anecdotal evidence suggests some women may feel very jittery or have anxious or racing thoughts while taking placenta capsules. It is recommended if you experience any adverse reactions to stop taking or reduce the amount of capsules you consume in a day.
If you are interested in placenta encapsulation or have questions regarding the practice of placentophagia, please feel free to contact me at meagan@beltanebirthservices.com!
Have you encapsulated your placenta? Or used a tincture? Made a placenta smoothie? I'd love to hear your experiences with placentophagia in the comments below!
If you are interested in placenta encapsulation or have questions regarding the practice of placentophagia, please feel free to contact me at meagan@beltanebirthservices.com!
Have you encapsulated your placenta? Or used a tincture? Made a placenta smoothie? I'd love to hear your experiences with placentophagia in the comments below!
Follow me on Facebook!
Questions about pregnancy, birth or postpartum life?
Interested in hiring a doula?
Please feel free to contact me
or check out my website!